A dog is an active animal. There is a good possibility that, as an owner, you will be faced with an emergency when your pet needs help before you can reach a veterinarian. If you prepare in advance by stocking a medical kit and learning the basics of what to do when danger arises, and if you remain cool in the face of crisis, you could be responsible for saving your animal’s life .
HOW TO RESTRAIN YOUR DOG
Often, because of restlessness or pain, an animal will refuse to cooperate when you’re treating an injury. It can easily be restrained by tying a loop of twine, rope, or cord around its muzzle and drawing the ends tight. Make a second loop beneath the muzzle and again cross or tie the ends and draw them tight. Then tie the loose ends behind the head to keep the loops from slipping off the nose.
Restrain a dog’s legs by approaching the dog from the side, grabbing the front and hind leg on the side away from you, and pulling the dog toward you so it is lying on its side. You are still holding the legs; this prevents the dog from gathering its legs under it and standing up. Carry a large dog from underneath, your arms around the top of all four legs. Hold a small dog with one hand under its chest; use the other hand to fold its legs underneath. If the dog is not cooperating, don’t attempt to restrain the legs without muzzling the dog first.

restraint

holding a small dog

holding a large dog
While transporting an injured dog to the veterinarian, you want to keep it from injuring itself further, or causing itself greater pain, by struggling. If a limb has been injured, immobilize it with a makeshift splint. Pick the animal up with the injured limb away from you, so that the limb will not press against you. Lift it with one hand under the chest, cradling its hind legs with the other. If you are sure there are no internal injuries, you can also lift it very gently under the abdomen. This way you can support it and, if there are any chest problems, it can breathe easily.
If an animal has been very seriously injured, is in great pain, or has a broken back, use a makeshift stretcher such as an ironing board. A blanket or towel is also an efficient stretcher and, because it confines the dog, prevents struggling. For this, you require two people, one to hold the corners at each end.
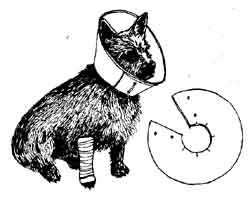
An Elizabethan or bucket collar made of cardboard is an effective means of keeping the dog from licking at wounds, biting its hindquarters, or scratching its face. This can be cut out of shirt boards or boxes. When you’ve slipped it around the dog’s neck, tie, staple, or tape the ends together.
THE INITIAL EXAMINATION
Unless you actually witnessed the accident and know exactly what the injuries are, your first job will be to inspect your pet rapidly and thoroughly, following this step-by-step procedure. These priorities are vitally important, for they are based on degrees of danger, in terms of how quickly action is needed.
RESPIRATION
Before anything else, check to see that your animal is breathing normally. If the brain is not receiving oxygen, this can cause irreversible damage, and even death, within four to five minutes.
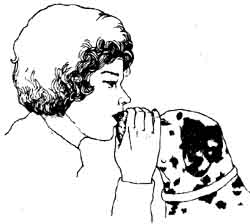
If breathing has stopped altogether, apply artificial respiration immediately. With the animal lying on its chest, cover its nostrils with your mouth and hold its jaws firmly closed with one hand. Blow steadily for two to three seconds, then remove your mouth for around three seconds to allow it to exhale before repeating. The volume of air should be enough to expand the rib cage normally. When the dog is breathing normally by itself, artificial respiration can be stopped.
Even though the dog may be breathing, is respiration normal? Is it taking slow, shallow breaths or rapid, short ones as though it can’t really expand its rib cage? Do you hear a gurgling sound when the dog inhales? This may mean free fluid in the lungs.
If an injured animal vomits or coughs up bubbly, frothy material, this may obstruct air flow. To prevent obstruction, raise the dog’s hindquarters so that they are higher than its head (at about a 30-degree angle from the horizontal) to allow drainage and to keep it from inhaling the material into its lungs. You can also do this by hanging the dog’s head over the edge of a table or the curb of a sidewalk, usually with the animal lying on its side.
If the dog is gagging or choking, move its tongue to one side and insert a small wedge, such as a roll of tape, between its jaws on one side. The wedge keeps the dog from biting its tongue and keeps the mouth open so air can move more freely. Take care not to put your fingers in its mouth, as an animal in pain will clamp down with all its strength.
HEART
Your second priority is to see whether your dog’s heart is beating. One possible and dangerous indicator would be blood spurting in pulses from a severed artery. If this is the case, go directly to the next step, External Bleeding.
Even though the heart has stopped, immediate external heart massage may get it started again, though if this doesn’t succeed within twenty to thirty minutes the animal will probably never regain consciousness. The dog should be lying on its side, with its head toward you. If you’re right-handed, its left side should be uppermost.
Place the flat of your stronger hand over the eighth rib, counting forward, the bottom rib being number one. It should be about two thirds down from the spine toward the center line of the chest. The flat of your other hand should be similarly placed under the dog’s chest, beneath the ninth rib counting forward. Apply a pumping action downward with the topmost hand, using the other to stabilize the dog’s body. The pace should be rapid, close to a pump every half-second, but use a steady pressure rather than beating or punching the chest.

If you have someone to help you, artificial respiration (described above) should be given simultaneously, timed to the heart massage. After five massages, allow one breathing cycle (one breath in, one out), then resume the massage.
During the heart massage, the femoral pulse can be monitored to make sure the pressure is strong enough to eject a good flow of blood from the heart. After any accident severe enough to require heart massage, a veterinarian should be consulted.
EXTERNAL BLEEDING
Your main concern here, from an emergency standpoint, is the possibility that major blood vessels may have been cut. If blood keeps soaking through the bandage as fast as you can apply it, a tourniquet will be necessary. Ropes, belts, stockings, or handkerchiefs can be used to make a loop around the limb. The tourniquet should be placed above the first joint of the limb, or at least four to five inches higher than the wound. Tighten the tourniquet by putting a stick, pencil, or a similar object through the loop and twisting it clockwise. Once the bleeding has been stopped, you will be able to get a dry bandage in place. If it is going to take time to reach a veterinarian, a tourniquet should be loosened, but not removed, for about a minute at intervals of ten to fifteen minutes.
If it is minor, a cut on a dog’s limb can be easily controlled by a pressure bandage placed directly over the wound. Three or four gauze pads, facial tissues, or napkins should do the job. These are then wrapped gently but firmly with a meshed gauze or Ace bandage, or makeshifts such as a nylon stocking or strips of old linen sheets. The wrapping should not be tight enough to stop circulation.
The bandage should be wound from the top of the leg down to the toes. With serious wounds, don’t waste time frying to clean them. All you want to do is to stop the bleeding until you can get the dog to a veterinarian.
When speed is not of the essence, the proper procedure for bandaging wounds is to first cleanse them with either hydrogen peroxide or Massengill’s douching powder mixed with warm water, or Betadine solution, flushing to remove all pus and debris. Then apply an antibiotic ointment, such as bacitracin, and protect the wound with a clean gauze dressing.

To apply a full bandage to a limb, follow these steps:
1. To prevent slippage, place two strips of 1-inch adhesive tape on the sides of the leg to act as stirrups.
2. Starting at the bottom of the leg, gently wrap thick, soft bandage until it is well above the wound, preferably as high as the next joint.
3. Cover this with gauze bandage. Wrapping the leg from the toe up will help prevent the toes swelling due to poor circulation, but the toes should be left exposed to be checked should any swelling develop and for signs of moisture accumulation.
4. Attach the two tape stirrups to the side of the bandage. Wrap the final bandage with 2-inch adhesive tape to protect against soiling and to give added strength.
5. Wounds on the head, chest, or body are often difficult to bandage. The only solution may be to hold a pressure bandage in place with your hand.
INTERNAL BLEEDING
Internal bleeding is a common result of car accidents or falls from high windows. You can detect it by examining the mucous membranes on the inside of the dog’s upper lip: they will have a cold pale color rather than the normal warm pink. Also check the pulse to see if it feels weaker than usual, flowing threadily rather than with firm bounds. Breathing will usually be more rapid than normal.
The spleen, kidneys, and liver are the most common sources of internal bleeding following accidents. The most obvious sign of this will be a fuller abdomen than usual. Apply pressure with a body bandage wrapped snugly around the belly. Strips of sheets, gauze, or Ace bandages can be used.
If you suspect internal bleeding, the animal should be jostled no more than is absolutely necessary to get it to a veterinarian. The best means will be to move it carefully on a firm support, such as a stretcher of plywood.
SHOCK
Shock itself, while it might be the result of other injuries, requires treatment. The symptoms are weakness, physical collapse, subnormal rectal tempera- hire, the pale cold appearance of the inside of the lips, listlessness, depression, fast but weak pulse, rapid, shallow breathing. There can be many causes, ranging from severe injury to electrocution.
If your animal shows symptoms of shock, wrap it in a blanket to keep it quiet and warm until a veterinarian can give it the care it must have for this condition.
The checklist above will assure you that you have done all you can, by yourself, to handle threats to your dog that require instant action to save its life. There are other situations, though, in which you can help your pet until it can receive the professional attention that is needed. Here are the things to watch for and what you can do.
THE UNCONSCIOUS DOG
Unconsciousness can be the result of a number of causes, from a blow to the head that causes concussion to a metabolic disturbance, such as hypoglycemia (decreased blood sugar), which often occurs when young puppies are unable to match their high energy demands with sufficient food to supply the necessary calories. The unconsciousness, a state of coma, may not be complete but will show up in a diminished response to a test such as a pinch on a toe.
Hypoglycemia occurs in puppies two to eight months old — it is an acute condition that can be prevented at an early stage if the puppy’s owner is alert to the possibility. Signs of mental slowness or difficulties in walking (staggering) are danger signals and the puppy should be given a teaspoon or two of maple syrup, sugar water, or honey every two hours until the condition is corrected.
Unconsciousness (total or partial) should always be brought to the attention of a veterinarian, for there are metabolic diseases other than hypoglycemia that require a veterinarian’s care. Among them are diabetes mellitus (high blood sugar), kidney diseases, severe uncontrollable vomiting, or congestive heart failure. (Do not worry about the sugar you gave your puppy for its temporary attack of hypoglycemia — diabetes does not occur in puppies.)
If your pet is in an unconscious condition, it should be kept as still as possible and, if it is going to take some time to get to a veterinarian, it should be turned over every twenty to thirty minutes to prevent congestion of the lungs on the lower side. Watch carefully for vomiting because the swallowing reflex may not be functioning and take the steps given above (under Respiration, in the section on the Initial Examination) to keep it breathing properly. Also, note the rate and depth of respiration in order to properly inform the veterinarian of the animal’s condition.
SUDDEN PARALYSIS
This is usually a case in which a dog, with no apparent head injury and completely responsive to its owner, loses partial or complete control over one or more of its limbs. This is most often due to acute injuries affecting the spinal cord and peripheral nerves of the body and limbs. Spinal cord injuries as the result of a protrusion or rupture of an inter-vertebral disk are most common with dachshunds and poodles.
The inter-vertebral disks act as shock absorbers between the vertebrae of the spinal column. If one should rupture, this may place a direct pressure on the spinal cord that results in paralysis of the limbs to the rear of that point.
While they may be caused by an accident, ruptured disks are more usually the result of strenuous activity that places too much stress on a weakened disk. Spinal cord injuries may also be due to tumors. Unless they are the result of congenital abnormalities or severe accidents to the spine, the causes of paralysis sometimes can be corrected surgically.
If your dog suddenly becomes paralyzed, take the following steps:
1. Place it on a firm support, such as an ironing board or plywood.
2. Move it as little as possible to prevent further damage.
3. Get it to a veterinarian as soon as possible. While this is not a minute- by-minute crisis, time reduces the chances of reversing the condition.
Other causes of paralysis not due to violent injury are:
TICK PARALYSIS. While the poison of one variety of wood ticks can cause acute paralysis, this is fairly uncommon and the symptoms will usually disappear once the insect is removed.
FAMILIAL NECROTIZING MYELOPATHY. This is a progressive degeneration of the spinal cord apparently inherited in certain lines of Afghan hounds. It often results in respiratory problems and inevitably results in death.
GERMAN SHEPHERD MYELOPATHY. A slow degeneration of the lower spinal cord characterized by rear leg weakness and unsteadiness that usually leads to complete hind limb paralysis.
MYASTHENIA GRAVIS. A neuromuscular disorder, which results in acute but short-term paralysis following vigorous exercise. The dog’s esophagus may swell and aspiration pneumonia is common, but the condition is sometimes controlled with the right medicine.
CONVULSIONS
The brain is surrounded by a certain level of electrical activity. Any interference can cause a “short circuit” with a discharge of impulses across the brain and throughout the central nervous system, resulting in a convulsion. There are many causes for seizures, among them distemper, viral encephalitis, lead poisoning, a scar defect resulting from past injury, and severe metabolic problems such as kidney failure and hypoglycemia. Epilepsy, probably the most common, usually occurs in dogs between three and five years old.
Regardless of the cause, a convulsive seizure will usually have three phases:
1. Pre-seizure — characterized by a dazed expression, sleepiness, unusual demands for the owner’s attention, hiding, and confusion.
2. Seizure — symptoms vary according to the site of the discharges from the brain. The animal may have only chomping mouth fits, or may have a full-blown grand-mal seizure, falling on its side and thrashing its legs about wildly, losing control of its bowels and urine, frothing at the mouth, and yelping. This may seem to go on for hours, but in reality usually ends in less than three minutes, often only seconds.
3. Post-seizure — this varies from dog to dog, but common signs are hiding, confusion, increased appetite, and sleepiness.
If your dog has a fit, you should immediately call the veterinarian and, while waiting, try to make your pet as comfortable as possible, keeping it out of harm, until the seizure subsides. Talking to the dog and stroking it gently will often have a soothing effect.
Do not try to prevent the dog’s swallowing its tongue by puffing your finger in its mouth. This is not a problem, as it is with humans.
Take some mental notes that will help the veterinarian in determining the cause of the seizure. How many seizures were there and how long did they last? On which side did the dog fall? Were there any pre-seizure signs? Has the dog forgotten any learned tricks, such as retrieving a ball, or has it been less responsive to commands lately? Has it shown any aggression to you, your family, or others recently?
If seizures continue to recur with increasing frequency, this “status epilepticus” can be fatal. The veterinarian uses a number of anticonvulsants — such as Valium, phenobarhital, and others — to control these seizures. While these don’t remove the cause, they reduce the chance of an attack. But even the best-medicated epileptic will have one or two seizures a year.
BURNS
There are three basic types of burns, caused by hot liquids (such as boiling water or coffee), chemicals (lye and sulfuric acid, for example), and direct fire or heat (perhaps from getting trapped under a car’s muffler).
How serious these are will depend on the depth, location, and surface area covered. Most bums are minor and require little treatment. The hair in the burned area should be clipped clean, for lingering infections are common under matted coats. Wash the areas of chemical burns generously with water to dilute the irritant. Other burns should be rinsed superficially with cold water once the hair is removed. Then apply a protective ointment — without rubbing the burn — such as Vaseline, or one of the many products made especially for burns; keep the dog away from it by covering the burn with gauze bandage (cotton will stick and impede healing), or by using an Elizabethan cardboard collar. This, and the bandage, can be re moved when the dog is no longer bothered by the burn.
If the burns are extensive, covering more than one third of the body surface, it is essential to take the dog to a veterinarian for immediate treatment.
HEAT STROKE
One of the most common problems, particularly in spring when the weather is changing, is heat stroke. Owners leave their dogs in the car while they shop, forgetting to roll down the windows, and apartments without air conditioning suddenly turn into infernos while the animal is home alone.
The dog’s only real source of cooling (it has sweat glands only oil its nose and the pads of its feet) is by respiration. With this handicap and a heavy hair coat, body temperatures can soar to as high as 110°F. The signs of heat stroke are rapid respiration and total collapse to coma, and often include vomiting blood and bloody stools. In such cases, take the following emergency measures:
1. Douse the dog in a tub of cold water or, if it is too large, spray it with a hose. In an emergency, rubbing alcohol can be used to lower the dog’s body temperature, but only with care, for if the temperature drops below normal this can throw the animal into shock.
2. Apply an ice bag to the dog’s head to prevent brain damage.
3. Cool the animal internally with cold water enemas or by placing ice cubes directly into the rectum.
4. Get to a veterinarian as rapidly as possible for fluid support and shock therapy.
FROSTBITE
Frostbite in dogs invariably affects the ears. Until the pet can be taken to the veterinarian to receive antibiotics, the essential step is to lubricate the ears with Vaseline or any other soothing ointment in order to protect them from infection, drying out, sloughing. Do not apply heat.
FRACTURES
If you believe your dog may have broken a bone, it should be taken to a veterinarian for an X-ray. Nevertheless, there are steps you can take to prevent further damage.
Once you suspect a bone in a limb has been broken, you should do your best to immobilize it. Until you can get veterinary assistance apply a splint -- a wooden stick, yardstick, newspaper, or cardboard. It should be long enough to hold the entire limb still. Keeping the leg as straight as possible, secure it from above to below the point of the break with bandages. Using the same sequence as with the bandage, add the splint between steps (2) and (3).
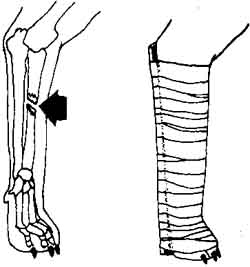
foreleg splint

hind leg splint
A fracture of the ribs, skull, spinal column, or pelvis is difficult to immobilize. In these cases, restraint is the best you can manage. The danger is a puncture of the lungs by a rib or a urethra lacerated by sharp pelvic bones. Use a temporary stretcher to take your dog to the veterinarian. In mature dogs, most fractures will mend in four to six weeks. The time is much less in young puppies.
DISLOCATIONS
The most common dislocation in dogs occurs in the hip joint. The ball, or head of the femur, in this “ball-and-socket” joint fits snugly into a depressed indentation of the pelvis called the acetabulum, which serves as a socket. Violent activity, whether in an accident or roughhousing, can pop this ball out of the socket.
Often the only way you can tell this has happened is when the dog starts to limp, trying not to put weight on the limb. Usually the toes will touch the floor; only rarely will the dog carry the leg off the ground. It should be taken to a veterinarian right away.
After X-rays eliminate the possibility of a fracture, the veterinarian may anesthetize the dog and try to relocate the joint manually. After more than twelve hours, muscle contraction makes this difficult and sometimes impossible.
Minor dislocations are quite common in poodles and Yorkies, and in these small animals are easily corrected. Shoulder, wrist, and hock dislocations are less common and can be detected by swelling and sensitivity.
BITE WOUNDS
How bad these are will depend on the sizes of the dogs involved, location of the wounds, and whether they are punctures or rips. Most are small and need nothing more than cleansing with a mild iodine or Betadine solution and application of a mild broad-spectrum antibiotic ointment such as bacitracin. Hot compresses placed on the wound for twenty minutes to half an hour, two or three times a day, will speed healing and lower possibilities of infection. The open wounds allow adequate drainage and promote healing from the inside out.
Small puncture wounds over which the skin has sealed can develop into painful abscesses because of the lack of drainage and the introduction of bacteria that infect underlying tissues. Extensive wounds may require suturing, drains, and antibiotics, which should be administered by a veterinarian.
SNAKEBITES
Nonpoisonous snakebites require little or no attention. The dog will show no more serious symptoms than mild localized swellings, a few hours of listless ness, lack of appetite, and lameness.
The pit vipers, such as rattlesnakes, water moccasins, copperheads, and coral snakes, which are found in some parts of the country, are another story. A commercial snake kit and sharp knife or straight-edged razor blade should always be available when traveling through areas where there are venomous snakes. Wounds inflicted by these snakes cause rapid, hot swellings, extremely tender and painful. If a bite is suspected, use the following procedure:
1. Apply a tourniquet between the wound and the heart if the wound is on a limb; this will slow the spread of the venom.
Loosen the tourniquet every ten minutes for short intervals. Most bites are around the face; a tourniquet, obviously, can’t be used then.
2. Apply an ice pack or cold water pack over the wound to minimize local tissue reaction, if possible. In addition to the swellings mentioned, there will be discoloration and tissue death. The toxin may also produce serious shock.
3. Phone a veterinarian immediately for advice.
As a last resort, if it is impossible to reach a veterinarian, use a sharp knife or razor blade to make a linear cut over each fang mark deep enough to cause free bleeding. If the puncture sites are not clearly visible, assume the wound is at the point of maximum swelling. Use a suction device, if you have one, to draw out the venom with the blood. Otherwise, do not use your mouth, but try to milk the venom out by pressing your hand down firmly on the leg below the tourniquet, stroking toward the wound.
INSECT BITES
Most often on the face, these can cause an acute generalized swelling of the muzzle, or a localized swelling at the site of the bite, which will usually subside completely within eight to twenty-four hours regardless of therapy. The best treatment is cold packs and ice placed o the wound for one hour. This is also true for bites and stings from black widow spiders, scorpions, and bees, which can be fatal. Deaths are usually due to acute allergic reactions. If a dog shows signs of weakness, difficulty in breathing, and pale mucous membranes in the mouth, a veterinarian should be called immediately.
POISONING
Consuming toxic plants or chemical intoxicants, or even physical contact with the latter, are the two major sources of poisoning in dogs. The effects vary widely, depending on the nature of the poison, the amount consumed, and the individual animal.
CHEMICAL POISONING. Almost every chemical has a toxic level in any living organism. The most common symptoms of poisoning include vomiting, diarrhea, drooling, shock, coma, convulsions, whining, and restlessness.
The basic approach to any poisoning should be the following:
1. Prevent further absorption of the poison.
2. Treat the poison specifically to aid its removal from the body.
3. Counteract the effects on the body with supportive care.
Many cities have poison control centers that can be called for specific information on potentially hazardous household products and their anti dotes. Your Department of Health can give you their telephone numbers.
The specific steps to take when your dog has come in contact with or swallows poison are as follows:
COMMON CHEMICAL POISONINGS IN DOGS
POISON |
SOURCE |
TREATMENT |
Amphetamines Arsenic Barbiturates Ethylene glycol Lead Organophosphates Metaldehyde Strychnine Thallium Warfarin (D-Con) |
Diet pills Herbicides Sleeping pills, sedatives Antifreeze Lead-based paints, linoleum, bird shot Flea, ant, roach, and tick sprays Snail bait Rodenticide Rodenticide Rodenticide |
Chlorpromazine Dimercaprol (BAL) CNS stimulant: Doxapram and Bemegride Ethyl alcohol Calcium EDTA Pyridine-2-aldoxime (2-PAM) and atropine Pentobarbital Pentobarbital Prussian blue Whole blood transfusions, vitamin K |
A FEW OF THE COMMON PLANTS POTENTIALLY POISONOUS FOR DOGS
COMMON NAME |
SCIENTIFIC NAME |
DANGEROUS PART OF THE PLANT |
SIGNS OF POISONING |
Dumbcane Philodendron English ivy Privet Tobacco Oleander Foxglove Lily of the valley Poinsettia Rhododendron Castor bean Daffodil Golden chain Larkspur Autumn crncus Daphne |
Dieffenbachia sequine Philodendron spp. Hedera helix Ligustrum vulgare Nicotiana spp. Nerium oleander Digitalis purpurea Convallaria majalis Euphorbia spp. Rhododendron spp. Ricinus communis Narcissus spp. Laburnum vulgare Delphinium spp. Coichicum autumnale Daphne spp. |
Stems Stems, leaves Leaves, benie Leaves, berries Leaves All parts Leaves Leaves, flowers Leaves Leaves Leaves, beans Bulbs Leaves, seeds Leaves, seeds Leaves Bark, leaves, fruit |
Salivation, laryngitis Salivation Vomiting, diarrhea Vomiting, diarrhea CNS stimulation Heart irregularities Heart irregularities Heart irregularities Heart irregularities Vomiting, diarrhea Diarrhea, shock Vomiting, diarrhea CNS stimulation Paralysis, CNS depression Vomiting, CNS stimulation Vomiting, CNS stimulation |
Induce vomiting. 1 to 2 teaspoons (5 to 10 ml) of hydrogen peroxide should work within three to ten minutes. Another less reliable method is to place a teaspoon of salt in the back of the dog’s mouth. CAUTION: Do not induce vomiting in the case of corrosive poisons ,such as kerosene, strong acids, or lye.
Protect the intestinal tract. When the dog has vomited, protect the stomach and intestines with 1 teaspoon (5 ml) per 5 pounds of body weight of Pepto-Bismol, aluminum hydroxide, Methigel, Maalox, or Magwol. Kaopectate should be avoided because it slows the intestinal tract.
Skin that is inflamed or irritated because of corrosive materials such as kerosene, gasoline, excessive use of mange dips, flea or tick baths should be rinsed with large amounts of water to dilute the irritant. Afterward, you may lather the animal gently with a mild detergent such as Ivory soap and rinse. Do not scrub.
If the dog shows hyperirritability and convulsions, quiet the dog and keep it from further injuring itself until a veterinarian can be reached.
Call your veterinarian about any poisoning. Get advice by phone and, if the veterinarian thinks it necessary, preparations can be made for receiving a poisoned animal. Take a sample with you, if you go, of the poison or the dog’s vomit. The best thing is the container with its label.
PLANT POISONTNG. The list of potentially poisonous plants is extremely long. Most are only in part toxic and symptoms will depend on how the poison works as well as the amount consumed. The commonest are copious salivations, vomiting, and diarrhea. Those affecting the central nervous sys tem may cause hyper-excitability, convulsions, paralysis, shock, and in some cases death. If you have pets that chew on house plants, it would be wise to find out which are potentially dangerous. In cases of plant poisoning, all you can do is induce vomiting (see above) and rush the dog to your veterinarian.
SMOKE INHALATION
This usually results from an animal being trapped in the vicinity of a fire. In severe cases, follow the procedures listed for artificial respiration and external heart massage. Then take your pet to a veterinarian.
Smoke inhalation can damage the epithelial lining of the respiratory sys tem and cause severe bronchitis or pneumonia. Even though the animal responds well to initial treatment, it may later suffer serious effects as a result of permanent damage to its lungs.
ELECTRICAL SHOCK
Teething puppies are frequently injured by chewing through electrical cords. Bums at the corners of the mouth are the obvious damage, but a puppy that has suffered electrical shock can also develop an abnormally rapid heart rate (atrial tachycardia) and there may be a very heavy buildup of fluid in the lungs (pulmonary edema), so it should be examined by a veterinarian. Both these conditions, if untreated, can be fatal. Once these possibilities have been dealt with, the pup may need to go on a diet of liquids and soft foods because of its painful mouth. Ointments should be applied to the bums.
EYE INJURIES
Eye injuries are common in dogs. Foreign material, such as a splinter, may become lodged in the eye’s surface. Interior damage as the result of a blow or puncture can result in a loss of the fluid of the cornea or the appearance of blood within the eye. The eye might even be torn entirely out of its socket. The first objective must be to get the dog to a veterinarian as soon as possible. Every moment is important. To minimize damage:
1. Place a wet paper towel or rag over the eye for protection and to keep it moist.
2. Comfort the animal to relieve its fear.
3. Get to the veterinarian immediately.
NOSEBLEEDS
Nosebleeds can be the result of injuries, but they may also be symptomatic of other problems, such as a nasal infection that has eroded the blood vessels, blood disorders, a foreign object in the nasal passages, or tumors. A dog with a nosebleed should therefore be taken to a veterinarian immediately, once the following steps have been taken:
1. Keep the dog as quiet as possible.
2. Apply an ice pack to the nose to reduce the bleeding.
Your veterinarian will administer hypotensive agents to lower the dog’s blood pressure and nasal packing soaked in epinephrine to constrict the blood vessels in the nose. These will usually bring the bleeding under control so that the problem can be diagnosed and any necessary further treatment prescribed.
FOREIGN BODIES
A variety of accidents can result in foreign bodies becoming embedded in one part or another of the dog’s anatomy. In most cases, so long as these are on the surface, no serious injury will result. An object under the skin will work its way to the surface, causing an ulceration as the body rejects it. Inasmuch as ulcerations can be indicative of other problems, these should be brought to the attention of a veterinarian. If there is nothing more serious, the ulceration will be treated for itself.
Objects embedded in the outer ear will follow the pattern above. If some thing reaches the inner ear, though, this is far too delicate an area for home treatment and should be treated as a medical emergency.
Symptoms indicating a dog may have swallowed a foreign object are vomiting right after eating, abdominal discomfort, restlessness, fever, and lack of appetite. The dog with any of these symptoms should be seen by a veterinarian.
The primary threat to the mouth and throat is bones. Even a needle, if it passes down the throat, is not necessarily cause for alarm. It can go through the dog’s digestive tract without causing harm. But bones and even some times balls may become lodged in the throat. This constitutes a full-scale emergency and the animal must be rushed to the veterinarian immediately. Any attempts at first aid may well result in even further damage. Speed is the only answer.
INABILITY TO URINATE
Inability to urinate is a medical emergency and the dog should be taken to the veterinarian immediately. This is rarely a problem with females but is not uncommon in males and is usually the result of objects that have become lodged behind the os penis, the bone in the male organ. Dalmatians are particularly susceptible to this as a result of uric acid stones.
The symptoms of urinary obstruction are an increased urgency to urinate, straining while doing so, and short, repeated squirts rather than a steady stream. The owners of males should be alert to these signs.